Summary of the argument
Evidence based medicine claims to be the paradigm for modern psychiatry. It represents proven treatments for defined diagnoses. But there are major problems with this position, starting with the fact that while they are superior to placebo, evidence based treatments too often are ineffective. It cannot be assumed that classifying psychopathology diagnostically is the best way to move forward. Established diagnostic entities, are as much wish as reality. DSM IV diagnoses are arrived at by committee decisions, by the convening of “experts”, with all that implies. Complicating the process is the fact that expert committee members can be influenced by pressures from those with an agenda, especially experts who receive a significant part of their income from pharmaceutical companies. The authors of DSM III and IIIr had it right. They also had to make committee decisions but they emphasized that their conclusions were tentative, so tentative that they weren’t willing to use the term diagnosis to characterize DSM designated illnesses. They were presenting operational definitions, with all the strengths and weaknesses this implies. In keeping with their scientific orientation, they insisted that the term “disorder” rather than “diagnosis” be used in the diagnostic manual. This starkly contrasts with the spirit behind the soon to be DSM V. “Evidence based medicine”, is being touted for its scientific prestige precisely as the process has forsaken the true spirit of science, openness about what is known and not known. Robert Spitzer MD, former chair of the work group for DSM III, has rightfully condemned the confidentiality agreements required of DSM V committee participants. 25 He wants detailed minutes of the task force’s deliberations, a no-brainer for those who understand the necessary tentativeness of scientific information, but problematic for those who want to provide an illusion of consensual certainty about diagnostic categories. There is also a more fundamental issue, not answerable to the vote of even the most “expert” committee.
What do diagnoses represent? Does every diagnosis in DSM IV represent an actual real illness, in the sense that polio, cancer, or a strept throat actually exist? Or can they represent the reification of an idea, taking diagnoses beyond useful limits? Evidence based medicine, it is implied, should monopolize clinical approaches. But at this stage the proper question isn’t should we exclusively use treatments that have proven superior to placebo? It is what is the best way to formulate treatment strategies when now, and in the foreseeable future, science can’t offer answers that we need? Conjecture, out of necessity, must play a significant role. Given mediocre treatment results, we need all the help we can get, the art of psychiatry as well as the science. Pharmacological agents can be viewed as inducing particular psychological states which, though not specifically related to diagnosis, are nonetheless the basis for their usefulness. SSRIs are efficacious in a broad range of conditions because increasing serotonin has a psychological impact that is nonspecific to the disorders. Many patients describe this as a “well whatever” state of mind. For this reason it can be used in treatment contexts when diagnosis is irrelevant (e.g. helping a picked on, thin skinned adolescent, develop thicker skin) The core issue is our approach to patients. Evidence based medicine eschews the anecdotal in the name of generalized conclusions, based on the odds that the patient’s ailments are typical for their group. This is not a ridiculous consideration, but it can miss important particulars brought by the patient. Knowing a patient well can be the difference between effective and ineffective treatment. Premorbid defenses, character style, the nature of the patients’ stressors, their story can guide clinicians to a particular medication, and influence dosage. While evidence based medicine has a place, especially when low cost is a consideration, it cannot lay claim to being optimal treatment. It is especially detrimental if this perspective acts like blinders, obscuring more than it clarifies.
*****
Evidence based treatments are presumably the gold standard. Each has demonstrated superiority to placebo that could not have been due to chance. Unfortunately, this doesn’t guarantee effectiveness. Even with treatment compliance, many patients do not return to their premorbid selves. Their ailment may last for years. A given percentage is not helped at all. Typically, 30-50% of depressed patients 1,2,3 will not respond, and among non-responders only 23.5-28% are helped by a second medication.4 The relatively common failure of evidence based treatments to achieve remission is not unique to depression. Frustrating both doctor and patient, similar results are found throughout the full spectrum of DSM IV disorders. This is not surprising. The science of psychiatry is still young, its conclusions necessarily preliminary. Psychiatry has not found its penicillin, a drug that will succeed 99 per cent of the time in eliminating strep throat, because it kills the germ causing the illness. DSM IV diagnoses are operational definitions, the best attempt by committees of experts to group manifestations of psychopathology into “disorders”. This cataloguing is not the same thing as understanding cause and effect. We haven’t yet discovered the etiology of any DSM IV diagnosis. The true fruits of science usually await this knowledge.26
Sometimes, psychiatric medications work as miraculously as penicillin. The patient returns a few weeks after beginning a medication and is amazingly restored. However, this doesn’t happen as often as we’d like, and when it does, we cannot always explain what has occurred. Neuropharmacology is a sophisticated science. Medication can be designed having specific effects on specific neurotransmitters. Extraordinary technological advances enable us to see what parts of the brain are effected by the drugs that scientists have designed. But, in contrast to penicillin, we don’t really know how various medications work with a given disorder. Our success rate reflects this. What is the clinician to do when the promised results of treatment are limited? He has no choice. Decisions about therapy must be made with or without needed hard knowledge. In a similar vein, there is a more general problem over and beyond inadequate efficacy for a given diagnosis. While researchers have the luxury of choosing patients who comply exactly with DSM IV criteria, in the real world of clinical practice, patients’ presenting symptoms are not always as cooperative. Whether a patient’s symptoms exactly correspond, or not, to DSM IV criteria, clinicians must treat patients as they exist. Otherwise they will be treating only a fraction of those needing care. Trying to remain within a scientific paradigm, once the first treatment (and perhaps a second or third) has failed, well-trained clinicians can become very “creative” when assigning a diagnosis. Presumably, once that decision is made, further treatment can be guided by evidence based protocols. However, reaching the documented 60-70% success rate for the disorder in question is unlikely since the liberties taken with diagnostic criteria leaves the clinician very far from scientific ideals. And this is not taking into account a different strategy, being guided by expert consensus protocols, treatment recommendations for a given diagnosis based on a polling of “experts” rather than empirical evidence.
In the journals these problems may be tackled in a similar way. Fuzzy diagnoses are encouraged by imaginatively broadening diagnostic criteria (for example spectrum disorders). Or new criteria are created, as has been done, for example, with bipolar disorder in children. This diagnosis has apparently captured the imagination of a good many practitioners. There has been a forty fold increase in this diagnosis over the course of a decade,6 despite its speculative nature. There is scant evidence that adult bipolar meds work for children. Nor is it known whether what is being called childhood bipolar disorder is the real thing (i.e. longitudinal studies documenting that these children are indeed at the beginning of a life long cycle of mania and depression) Those advocating newer broader criteria for what constitutes a disorder may reasonably argue for broadened diagnostic criteria in a future DSM V. The expanded diagnosis may indeed represent progress, forwarding our understanding of a given disorder. But, all too often, new scientific knowledge is not the basis for the expansion. It is the need to find a diagnosis so as to adhere to a science based protocol, even though scientific reliability has been necessarily violated by a loose application of diagnostic requirements.
Besides controversies about specific diagnoses it is useful to step back and reconsider what, at first glance, seems like a simple issue. What do DSM IV diagnoses represent? As already noted, when DSM III, and later, DSM IV were released, the authors acknowledged the distinction between diagnoses based on etiology or pathophysiology, and the operational definitions APA committees of experts voted on. Operational definitions have a specific purpose in research. Amidst uncertainty, they allow researchers to move forward, confident that they are talking about the same thing. On the other hand, not paying heed to this issue, assuming that DSM IV diagnoses are more than they are, reifying them, can lead to conclusions that make no sense whatsoever, when viewed in the light of later understanding of what is actually occurring. To illustrate, let us consider congestive heart failure (CHF) as a model. An important aspect of CHF treatment is to focus on a manifest symptom such as edema, especially pulmonary edema and pleural effusions. The strain on the heart from excessive fluid demands the use of diuretics (which, of course, do not act on the heart but on the kidneys). Unencumbered by fluid in the lungs, shortness of breath and orthopnea will improve. Treatment addresses pathophysiology without taking etiology into account. The actual diseases that brought about the heart failure are once removed from the focus of treatment. Heart failure might be due to muscle damage from an MI or a viral cardiomyopathy. There might be valvular damage from rheumatic fever, or subacute bacterial endocarditis, and so forth through a long list of diseases that can damage the heart. A clinician focusing on the presenting symptoms of CHF is proceeding rationally because regardless of etiology, when the heart doesn’t do its job–when it is not pumping blood powerfully enough–the final common pathway manifested by the accumulated fluid may be of more immediate concern than the underlying cause of the illness. One hundred years ago CHF could be described without an understanding of its many causes, and that description remains therapeutically relevant today, even after we can now better understand underlying causality. But there is a problem illustrated by CHF as a diagnosis, which is relevant to the way we use DSM IV today.
For argument’s sake, let us say our knowledge base remained at the turn of the 20th century and hypothyroidism was causing the heart failure of a given patient. Thyroid extract would fail miserably when tested in a larger population of patients whose “disorder” had been defined as “congestive heart failure.” It might worsen in particular, the illness of those patients whose CHF was, for instance, caused, or exacerbated, by atrial fibrillation due to hyperthyroidism. Viewed from the perspective of the heart failure diagnosis, the few patients it helped might be described in individual case studies, but would be rightly dismissed as anecdotal, if proponents argued that it should be used as a general treatment for congestive heart failure. Yet, the fact remains that it is exactly the correct treatment for CHF due to hypothyroidism.
My point is obvious. As reasonable as evidence-based treatment protocols for symptom-defined “disorders” might seem to be in psychiatry, they can be nonsensical compared to what is possible when a true understanding of etiology can be used to provide rational care. Analogous to CHF, schizophrenia might be 5 or 7 or 12 different diseases all with the same common final pathway. The heart is basically a pump. Thus, many different illnesses can manifest themselves as the same “disorder” when its pumping action is defective. Similarly, there may be limited numbers of ways that the brain can malfunction when its higher integrative functions are not working properly, or are overpowered by extremely forceful primitive emotional currents. There might be a genetic-caused schizophrenia-like illness with 100% (or 25%) penetrance, a virally based illness, nutritional etiologies (besides known vitamin deficiency induced psychosis.). Some have suggested fetal damage. There might even be (dare I say it) an illness primarily caused by detrimental child rearing. At one time, a syphilitic psychosis resembling schizophrenia used to fill up mental hospitals, so let us not ignore bacterial causality. And what will we learn about prions?
The point is that any number of diseases sharing common symptoms could mistakenly be lumped together. It is an inherent shortcoming of any system based on symptoms alone. Each of the DSM IV disorders could be several illnesses that appear similar to each other but are, nevertheless, not the same illness. Indeed, a person with no symptoms at all might be a closer match to a person with symptoms, than someone with very similar symptoms. For example, we now know that someone with early latent syphilis (two years in to the disease) showing no signs of illness (once again, for arguments sake, before VDRLs were available) should be treated for the disease regardless of symptoms. Someone with optic neuritis (a common manifestation of neurosyphilis) who is not infected by treponema pallidum, would not be helped by penicillin. There is nothing perplexing here. Our understanding of cause and effect allows clear thinking. Families with schizophrenia running through them have an abundance of schizotypal disorder.5 Once again, not a surprise; some day in the future we might find certain patients now diagnosed with panic disorder, or obsessive compulsive disorder, appropriately grouped, from the standpoint of etiology, with some schizophrenics. On the other hand, someone with a biological predisposition, say, towards excessive fearfulness (anxiety), or passivity, might have manifest symptoms that veer towards phobias, avoidant personality, obsessive compulsive disorder, panic disorder, or any one of a number of DSM IV disorders, the differences between them attributable to family or culturally learned defenses, parental models of coping, individual trauma, or individual psychodynamics. For example a person using counter phobic defenses (say sky diving) to “choose” and attempt to master their risks for themselves, will present very differently than a frightened individual passively yielding to that fear, or trying to gain a sense of control through repetitive OCD rituals, or dependent on the protection of others, or on idealized love, or through submersion in cults. And medications that treat “anxiety” might be helpful in a large number of disorders that vary greatly from each other in manifest symptoms, but might have in common the fact that the particular symptoms (shaped by other factors) were fundamentally a response to genetically based greater quantities of “fear.” Are they all the same disease, or as some would have it, are they part of a spectrum? Using the common effectiveness of a given treatment might give hints about etiology, but, not necessarily. Syphilis, pneumococcal pneumonia, and strep throat, are very different diseases, with symptoms that do not resemble each other, but they are all bacterial and are all handled very nicely by penicillin, just as SSRIs are effective for all kinds of different illnesses.
To play with the analogy a bit more, strep throat is not really the same disease as rheumatic fever, although the same germ is involved in both diseases. The key point is that current DSM IV disorders are not likely to be equivalent to each other as separate, equal diagnostic entities once we understand the complexity of their underpinnings. That there are gray areas in making a diagnosis is perfectly legitimate. I suppose the fear of those opposed to putting diagnostically centered psychiatry aside is the slippery slope of not classifying patients with psychopathology as suffering from “illnesses.” The concept of spectrum disorders is theoretically legitimate as an attempt to remain with a diagnosis paradigm, but it too introduces a slippery slope in the application of the idea. The problem may be that,at some point, making a diagnosis is not adding either understanding or scientific validity. It is going through the motions, staying with familiar approaches even if it may no longer make sense, because it seems “scientific” to do so. Implicit in the decision to stretch the diagnosis, to include a patient that doesn’t meet criteria for that disorder, is the belief that the disorder exists in the same sense as an infection or tumor or diabetes. It is not just an operational definition. It is real in the same way as say, a child presenting with fever, achiness, vomiting and diarrhea, without complaining of a scratchy throat, may nevertheless be suffering from strep throat. A clinician who claims a child or adult “really” has bipolar disorder, or ADHD despite not meeting defined criteria, assumes something is going on related to their actually having a specific disease process. Something is wrong with their brain circuitry, or neurotransmitters, or genetics that justifies the diagnosis even if it isn’t presenting itself in the usual way, or cannot be demonstrated. And a medicine is going to be effective because it somehow attacks the fundamental pathological process.
While clinicians sometimes succeed when they try one medication after another on a trial basis, justifying this by a series of guesses about the “real” diagnosis, attributing a diagnosis doesn’t necessarily add to treatment success. Since, for the most part, we do not understand how the medications work for a given diagnosis, we haven’t added very much to our approach. The problem of reifying diagnoses extends beyond trying to classify patients who don’t meet full DSM IV criteria. Some disorders are problematic not only because they are spectrum extensions of a diagnosis. From a common sense perspective the cluster of symptoms defining the “disorder” is unlikely to be a disease, as that term is commonly understood. For example, it is possible to operationally define the cluster of symptoms that constitutes oppositional defiant disorder. While certainly something is troubling about the behavior, and in theory it may be studied objectively, is classifying this a “disorder” necessarily the best way to conceptualize it? Merely labeling a syndrome of behavior a disease creates problems. Here is a quote from Educational Horizons Spring 1996: “Once upon a time parents who lacked the courage and/or interest necessary to set limits and impose responsibilities were thought to produce lamed and defiled children. “Spoiled brats” was the common lexicon. Happily, this benighted notion no longer enjoys currency. We now know that a child’s upbringing may really have little to do with “brattiness.” Children behaving like “spoiled brats” are often really suffering from an illness known as oppositional disorder.”
Is this what we meant to do? Are we really going to solve the problem of oppositional and defiant children by calling it an illness? Are doctors “experts” in this area? Any parent who has raised a child with minor or major problems, knows that understanding their family’s and children’s issues in its specifics is more likely to bring results than the crude portrayal that emerges from the use of the broad brush strokes of diagnostic perspectives. There are more subtle issues. Obsessive compulsive disorder seems to have the characteristics of a distinct disorder and certainly thinking this way about certain patients can be helpful. But is OCD necessarily an illness or a way that the psyche handles unsettling issues. Its incidence varies in different cultures, most likely due to upbringing. The frequent(though not universal) preoccupation with getting clean, fear of germs, particularly from the toilet, points in the direction of Freud’s ideas about anal conflict. The fear of autonomy, the self doubting, the preoccupation with rules seemingly slavishly obeyed,(but passive aggressively resisted) the subjective experience of tiredness resulting from this continual struggle invokes Erickson’s description of the developmental stage autonomy vs shame and doubt.
All argue that we cannot reduce this disease to a serotonin imbalance. In the first place anything that gives relief from fear and uncertainly, yes serotonin but also morphine (Franz, 2001) can help symptoms . Indeed I had a patient who completely lost his symptoms after he had a religious conversion. Joining the Jehovah Witnesses wiped away his guilt. His return to innocence was accompanied by removal of his sense of impending doom. Now he was in God’s hands, whom he totally trusted in way that he could not trust himself, or any human being. He didn’t need to perform acts of contrition (or superstition) to free himself from his prison of fear and guilt. Of course the symptoms came back when he became disillusioned with the Jehovah Witnesses, but the fact that psychology not chemicals worked for this disease calls into question simple disease formulations.
And let us not leave out a completely different set of circumstances. I’ve had two patients that only had OCD symptoms when they were in a depressive phase of their bipolar disorder. Lithium got rid of the OCD. So did a manic phase, when all sense of uncertainty disappeared. Yes we can list OCD as a comorbid diagnosis in cases such as these but is this necessarily the best way of conceptualizing what is going on? Another illustration, (this time concrete and obvious) of how using the evidence based model distorts and blurs our reasoning can be found in the use of Herceptin for those breast cancer patients who have too much HER2 protein. Herceptin does nothing for the others. Statistical studies of its efficacy for all breast cancer patients would be meaningless if everyone with the diagnosis were studied. Similarly, the evidence based treatment model (based on diagnosis) can lead to cruder than necessary formulations as illustrated by the finding that Risperidone is effective for major depression when added to standard antidepressants treatments.7 Is this due to decreased anxiety in an agitated depression ( since anxious depressed patients don’t respond as well to treatment8 )? Or is there an inherent antidepressant quality possessed by Risperidone? If there isn’t an antidepressant action per se, would Risperidone be as helpful for a depressed patient with anergia or hypersomnia or psychomotor retardation? Or, would it make things worse since its antianxiety qualities are related to sedating properties? These important question are not addressed by the research because the study design is locked into the evidence-based model of efficacy for a diagnosis rather than the alleviation of specific symptoms. (It is noteworthy that the FDA is locked into this same diagnostic perspective as part of what it considers its all important function of designating treatment indications for a given dignosis. Legalistic criteria are the priority rather than true science, with its never ending desire to understand cause and effect) There are many other problematic issues to raise about evidence based medicine’s reliance on diagnostic psychiatry. However, we will leave this topic in order to return to the main point of this paper, that as laudable as a scientific stance is, we should unapologetically acknowledge the obvious. The inadequacy of our hard knowledge means clinical psychiatry is, and for the foreseeable future will remain an art as well as a science. There is value in formulating treatment rationales that are not statistically validated protocols based on diagnosis, but are, nonetheless, sensible.
The use of medications within a psychological/ clinical context paradigm as opposed to a strictly diagnostic (evidence based) perspective
Herman Van Praag’s classic “Nosological Tunnel Vision In Biological Psychiatry. A Plea For A Functional Psychopathology” (1990)9 warned that exclusively focusing on diagnosis can blind clinicians to other useful ways of approaching patients’ difficulties. Many clinicians limit their focus almost exclusively to the treatment of DSM IV defined symptoms. The rest of the patient’s complaints may be considered chaff, and therefore, shouldn’t be a treatment concern. With this perspective, fifteen minute, once a month med visits, may be all that is needed. However, as will be seen, this may not be optimal care, even if it is the treatment recommended by “experts.” It isn’t only frills we are addressing. A broader view of patients’ problems may yield more informed use of medication. Clinical context can be just as, or more important, than diagnosis. To illustrate this it will be necessary to repeatedly resort to what is commonly dismissed as the anecdotal.
Mr. T., a thirty-year-old man, unhappy in his marriage, had always pictured a family life with two or three children. His wife, a beautiful woman, whom he had originally been smitten by, had never wanted kids. Mr. T assumed she would change her mind. But now, six years into the marriage, he understood that there would be no change of heart. She was to be the project of the marriage, her vulnerabilities, her needs, the vicissitudes of her emotions. It had gotten old. Over the years, he had noticed his impatience with her grow into indifference and then sarcasm. He came for help when he had become depressed. He couldn’t sleep. He couldn’t eat. He couldn’t concentrate at work. Constantly running through his mind was how trapped he felt in his unhappy marriage.
I’ll put the issue in a nutshell. What if an antidepressant worked like a charm and completely rid him of his depression? What if it returned bounce to his life and now he found he could, after all, live happily with the status quo? This is, in fact, what happened. As long as he remained on an SSRI he was fine. But here is the key question. What if 25 years from now, Mr. T. were to wake up and realize he had wasted his life? He really had wanted children and a family all along. What if he wouldn’t allow a doubling of his SSRI dose at that point? A drug had deceived him, cheating him of what had been meant to be. Would Mr. T. have had major depression if he weren’t biologically predisposed? We don’t know. (Nor do we know with others.) But even if he would not have gotten as depressed without having a biological predisposition, it is wrong to dismiss his marital situation as merely a precipitant. In this case, his misery was an alarm signal. Depression represented his true feelings that the life he was living was making him very unhappy A further question: would a different antidepressant have led to a different conclusion about his marriage? SSRIs are excellent at turning off the alarm system. Respite from overwhelming emotions may have something to do with healing and recovery. The depressed person is no longer being overloaded with the experience of helplessness, a demoralizing sense that nothing the patient can do will matter. The question for us is would a dopaminergic, or adrenergic drug have led to a different idea about the marriage? In rats, when confronted with the hopelessness created in the FST (forced swimming test) those on SSRIs will do better than rats being fed placebo. They won’t give up as easily when faced with the impossible. Those on desipramine, interestingly, will more often try to climb out of the threatening environment.10
Ms. B. was having an affair with a married man who was on fluoxetine. When he came off his medications he couldn’t stand his marriage for a moment longer and he intended to marry Ms. B. As soon as he was back on meds his concern switched to his teen-age daughter who needed him to stay.
Which was the true judgment? Among my patients on SSRIs some have found the courage to ignore their fear of loneliness and leave an unsuitable marriage. Others found the courage to have what proved to be an unwise affair that devastated their family. The ramifications can get complicated.
On an SSRI Mr. Q, a 27 year old car mechanic with an Ivy League degree, decided to quit his 9-5 job as well as his part time band (which all along he had considered not up to his talent level). He planned to use his inheritance and “go for it” as a singer. Was this realistic? I suppose it depends on his talent, connections, and luck. He had previously been cautious about his inheritance (one million dollars from his grandfather) recognizing that it was a one-time thing and was his only hope for financial security. He felt guilty about receiving the money. ” It was unfair to others.” On medication this no longer applied. One of his original complaints, his social phobia, which was particularly paralyzing when he was attracted to a woman, had not been cured. However, he was no longer depressed and suicidal during weekends when he felt most isolated. He said he had come to realize that he could be content without people. Perhaps his contentment was helped by a significant drop in his libido, a great relief for this well brought up young man, whose trips to pornographic sites on the internet left him feeling even more ashamed than when he tried to overcome his shyness, and was rejected after he tried to initiate sexual contact on a date.
Only after Mr. Q decided he was going to use his inheritance to develop a solar car did I feel forced to act. He was not manic or hypomanic. He was calm and sleeping well. But he was about to gamble with his future financial security, possibly on the basis of a drugged state. When advised he would have to stop the SSRI, so that he could review without medication his solar power car investment, he stopped therapy and went to a different doctor.
Van Praag argued that pharmacological agents can be viewed as inducing particular psychological states which, though not specifically related to diagnosis, are nonetheless the basis for the usefulness of the medication. As an alternative to a chemical imbalance paradigm, which hypothesizes that inadequate serotonin is a key factor in an assortment of psychiatric illnesses, a case can be made that SSRIs are efficacious in conditions as disparate as borderline character, depression, obsessive-compulsive disorder, anorexia nervosa, panic disorder, social phobias, and so forth because increasing serotonin has a psychological impact that is nonspecific to the disorders in question. Alcohol will produce inebriation in a person with schizophrenia, obsessive-compulsive disorder, depression, or someone with no psychiatric diagnosis. Analogously, SSRIs typically impact individuals in ways that are not specific to diagnosis. What is that effect? Normal guinea pig and rat pups in the laboratory loudly squeal (emitting stress induced vocalizations) when separated from their mothers. If given SSRIs these vocalizations are reduced.11 The most frequent description of the effects of SSRIs that I have heard from patients are “It doesn’t matter.” or “Don’t sweat the small stuff.” or “What’s the big deal?” It is this “Don’t sweat the small stuff” perspective that I believe is SSRIs unique blessing and curse. It means relief from worry, relief from the feeling that something is missing, something needs to be done, something needs to be fixed, “my makeup isn’t right, the sky is falling, I won’t be able to pay my bills, I’m not smart enough, I won’t be able to tolerate the loneliness if I leave my lover” (even if he/she is abusive). SSRIs supply, if not always happiness, then a nice contented feeling that all is well and will be well. They can allow parents to be able to play with their children more, fret less over the details, appreciate what is, actually want to do the proverbial modern mantra, stop and smell the roses. On the other side of the equation consider this:
Ms. D became pregnant while successfully being treated with an SSRI . Despite misgivings, she decided to marry the father of her unborn child. Several years later, the patient now divorced, and again depressed, returned for treatment. I suggested an SSRI. She would not consider it. She blamed the SSRI for her original poor decision to go ahead with marriage. A psychiatrist colleague took fluoxetine to relax on her vacation. It worked so well she tried it at home when she returned. She quickly stopped it when she found herself thinking, “Who cares?” when her patients described their problems. Pomerantz 12 describes a patient that was getting speeding tickets while on an SSRI and similarly didn’t seem to be bothered.
According to this theory it is the “well whatever” feeling, emotional blunting, that is so useful in the great variety of different syndromes. Thus, for a person with anorexia nervosa to react with “well whatever” after they have gained a pound or two gets at the heart of the problem. The same can be said for body dysmorphic disorder, when imagined, or slight, body defects no longer seem important. In obsessive-compulsive disorder, the ability to treat compulsions and obsessional thoughts in this manner is a godsend (which interestingly is similarly helped by morphine13 a non-serotonergic med but which creates an even stronger but comparable mindset) Similarly, a depressed person’s preoccupation with the hopelessness of their situation, the gravity of their errors and defects, and so forth will be enormously relieved to regain a less “negative” perspective. In panic disorder, a condition characterized by exquisite sensitivity to body sensations, and a catastrophizing of consequences (a patient described an attack of terror after she feared she was losing her vision and only later, when she removed her glasses, did she realize that her dirty eyeglasses had set her off), SSRIs have been found to be effective because the sense of imminent catastrophe leaves. For similar reasons social phobias and bridge phobias and flying phobias often become manageable on SSRIs, as do intermittent explosive disorder which may improve because it is harder to press the patient’s button.
Alcoholism, pathological gambling, overeating and the like may respond if a sense of frustration has significantly contributed to the pathological behavior. (these conditions can worsen if a disciplined battle is being waged against temptation, which is then weakened by a “well whatever” letting down of the guard). SSRIs can help perfectionists (“obsessive compulsive personalities”) give themselves a little (or a lot of) slack. They can allow borderline personality disorder patients to cool off, to not be tortured, like a wounded lover, when the person, upon whom they have passionately centered their survival, is not reciprocally involved with them. And so we can apply this perspective about SSRIs down a long list of DSM-IV defined disorders that have been empirically found to be treatable by a change in brain chemistry. This perspective also suggests itself as useful in psychological circumstances where a specific DSM-IV diagnosis is not at issue. Thus, for instance, a not uncommon treatment scenario is teenagers who are having a very rough go of it with their classmates, kids who are picked on precisely because of their vulnerability. The popular students are the ones who are cool; that is, they don’t blush easily, are bold with the opposite sex, and so forth. Adolescents often turn to illicit drugs (analogous to adults at cocktail parties), to get rid of their social anxiety. What they are up against can be far more traumatic than what adults’ face, who more often gossip without the criticized person present. By contrast, teenagers may be extremely up front in social situations, meaning they delight in publicly torturing the nerds. It is not unusual for adolescents to come to therapy because they feel like misfits and to put it bluntly, the use of SSRIs may help by providing a thicker skin, which is exactly the quality they needed all along to not get picked on and possibly even have the “cool” to be “popular.”
How does that differ from drugging oneself out of problems rather than “learning critical skills during the formative years? Isn’t discomfort often a stimulant of growth, (the stutterer who becomes the grand public speaker, the short guy who becomes Napoleonic)? I’m not sure it is different, but that discussion will have to await a different article. The fact is however, that SSRIs are used exactly in this way and a myriad of other analogous ways by clinicians to the tune, according to one estimate, of 65 million people in the United States since their introduction. Right now, when they are found effective, a diagnostic perspective leads to the conclusion that the patient must have “really” been depressed, or has a subclinical version of an illness, or has a spectrum disorder. I am suggesting we can spare ourselves this pseudo logic and address the real question. Should we or should we not drug people into subjectively improved states when an officially designated “illness” is not at issue?14 As implied above, there are other perspectives that may lead to treatment success, characterological qualities that may guide our treatment, conflicts causing depression or anxiety, or mood instability, situations that may be highly relevant not only to psychotherapy, but more to the point, to the choice and timing of medications.
Mrs. L. had originally required hospitalization and 40 mg of paroxetine to recover from a postpartum depression. It worked well, but after seven months on the meds, an incident happened which disturbed her. During her lunchtime she was visiting her infant at his daycare center when one of the workers began screaming at another infant without picking her up. The next day Mrs. L went shopping during her lunch break. Later that week a coworker became tearful during the course of a conversation with Mrs. L. regarding her own child’s daycare center.
Only then did Mrs. L. wonder about her decision to go shopping the day after she had witnessed the daycare worker’s inappropriate reaction. She wondered if her paroxetine had made her indifferent, when ordinarily she would have reacted and worried about such a thing. Paroxetine was reduced to 20 mg. On less medicine there was a dramatic change in her perspective about many things. For the first time she spoke about the pressures she had been under at the time of her original hospitalization. Mrs. L. had tried to find time to be the powerhouse worker at her job that had brought her so many promotions in the past, an ideal mother for her newborn infant, and responsive to her husband’s very exacting standards about her housekeeping. Suddenly, without the higher doses of paroxetine, her fury poured out. She described, in detail, episode after episode in which her husband stood to the side and supplied her with a never-ending critique of her adequacy as a mother. The higher doses of medication had muted her responsiveness, allowed his criticism to go in one ear and out the other, but now there would have to be change “or else”. Mrs. L. also acknowledged that she had not been doing her job as carefully as in the past and eventually the company would discover her drug induced “what the hell” attitude. At home, she had bounced several checks, something that had never happened before she was on medication. Therapy now turned to how her life would have to change. She seriously considered stopping her job. She loved being a mother and didn’t want to miss out on her son’s crucial early years. She demanded changes in her husband (with the threat of divorce). Her new assertiveness had rapidly put him on good behavior even before marriage counseling started. A few times, during her sessions, she became tearful about her dilemmas. Although we discussed the possibility of returning to higher doses of medication should the need arise, she was not eager to do this. She felt her tears were about real things and did not consider herself depressed. She did not feel hopeless or helpless. Her sleep was not as restful. She sometimes tossed and turned. But she was okay.
We joked that we might go up on the paroxetine temporarily if, and when, she needed a vacation from her stresses. In fact, throughout I was concerned that her greater emotionality might be a prelude to the return of her original symptoms. But this perspective was quite different than an automatic increase of medicine at the first sign of tears. As it happens she did not need to return to a higher dose. She did quite well, eventually deciding to work part time. Three months after making that decision she was the happiest she had been in years. It is noteworthy that when, at her urging, she was reduced to 10mg there was another improvement (depending on perspective). She again noticed dust on her furniture. She noticed that the pictures on her table had been placed haphazardly. She arranged them more aesthetically, which is what she had done before SSRI treatment. She did not feel driven to take better care by the internalized monster described in obsessive personalities by Shapiro in “Neurotic Styles”,16 by an unending “I should, I should I should.” She took pride in her newly regained “attention to detail.” She also regained a degree of empathy for her husband. There certainly was the danger that she was returning to a dynamic of taking care of everyone and everything, of offending no one, a role that she had assigned herself from early on in childhood. This pattern may have played a part in her original postpartum depression as she tried to juggle her responsibilities and became overwhelmed, consequently generating forbidden anger at her newborn. Certainly, her regained empathy for her husband might be the beginning of permission for him to begin carping again but she thought she “would be able to handle that.”
The other issue that can be gleaned from these clinical vignettes is evaluation of proper dosage. If we stick to a strictly DSM IV symptom checklist, fewer and milder symptoms, are an absolute good in terms of the risk/ benefit ratio. While this perspective is often proper, with Mrs. L there was a downside to SSRIs as well as an upside. The dulling of emotions such as panic, anxiety, helplessness, uncertainty, feeling uncomfortable in social situations and so forth are indisputably good. It allows patients to get off the emotional roller coaster that psychiatric symptoms often represent, and puts them back in charge. This dulling issue would not necessarily qualify as a side effect, unless it became an inappropriate degree of indifference to consequences developed (as seen in mania, hypomania or as illustrated by Pomerantz’ case of the patient who was indifferent to speeding tickets). Yet, less dramatic effects on a patient’s fear of consequence, can still have importance in the patient’s life. What about a bookkeeper, or the architect of a bridge, or an engineer who has been driven by anxiety to produce perfectly executed calculations? What about a mother-in-law who is barely sensitive to her son-in-law’s feelings, but now medicated, and more relaxed about consequences, has her say. (Of course it is also possible that on meds she might be less sensitive to her son-in-law’s shortcomings.) If the above observations are correct, the qualities we are describing are inherent in this class of drugs. In other words what is good about them is what is bad about them. The evaluation of clinical appropriateness is not invariably related to diagnosis or symptoms, or the usual side effects. We are entering layers and layers of evaluation that psychiatrists may not consider their role. Certainly they cannot accomplish this in 15 minute once a month visits. Yet, if choosing proper dosage is an important function of psychiatrists, shouldn’t these more subtle considerations be part of delivering optimal care?
Shouldn’t experts address these issues? When our patients are making critical decisions about their life, while on SSRIs, is it good or bad to be under the influence? Increasing self esteem, or lowering fears of consequences (such as loneliness or rejection) may be a good thing for someone stuck in a bad marriage or job and afraid to make changes. Indecision can reach total paralysis in severe depression when self-esteem is fractured and fears of consequences are gravely multiplied, so here symptoms are clearly distorting the ability to act. The same can be said when mania leads to the opposite, reckless impulsivity. But, in the real world, these issues are often a question of degree and medication can be a complicating variable.
Ms. D a computer consultant, with a terrible foster home childhood, was successfully treated for depression with an SSRI. She had never felt she was as good a techie as her 4 male partners. She had a never-ending need for reassurance, which was embarrassing to her. It was part of the reason she had gotten involved in a number of foolish affairs. Every night on her drive home she tortured herself with the things she felt she had mishandled. On an SSRI all of this changed. She acknowledged that she wasn’t as good a techie as her partners, “but she wasn’t bad.” More importantly, she realized she was indispensable to her team. She was the only one with sufficient social skills to handle their clients. For the first time in her life she was able to ask questions at conferences without feeling like an idiot. No longer hungry for confirmation she was also able to stop her cycle of love affairs. On the other hand, her comment coming off meds was noteworthy. “I feel like I’ve been drugged for two years. Now I want to take a look at my checkbook.”
She also reported behavior that now, off the meds, seemed bizarre. She had bought a puppy that she kept in an unfinished basement. While medicated she had not cleaned up the poop, reacting with “well whatever.” Off the medicine she was shocked by her behavior.
Mr. K., a patent attorney for a large corporation, was overwhelmingly depressed at home and work. He had been depressed once before. The apparent cause was a difficult supervisor at his job. Almost daily, his supervisor would criticize some aspect of his work and Mr. K. would be immobilized for the rest of the day. Sometimes he would stare at the wall in a daze… “my father always called me a complainer…you don’t have to love your job; you just have to get it done… I’m a loser … those years in law school– all for nothing…” Placed on an SSRI Mr. K. was quickly fixed. His supervisor would enter his office, make his usual derogatory remarks and nothing would happen. Mr. K. returned to working productively.
There were other benefits. His overweight wife lost 35 pounds. For the first time in years, Mr. K. put down the TV remote control. They began having good conversations, the kind of talks they used to have when their relationship was fresh and engaging. Everything became new. Mr. K. realized that for years he had been going out on Sundays because he was irritated by the tumult of his children. On his SSRI, he found himself playing with his children and having a great time. After ten months on the medication we decided to see how he would do without it. Within a few weeks we were back to square one. His supervisor’s remarks were again devastating him and he was a grouch at home. He made a quick recovery once he was placed back on the medication. After 16 months on the SSRI Mr. K. found a new job. He loved it. He came off the meds. He did fine. There were only a few peculiarities that he commented on when he got off the medication. Although overall he had worked far more effectively on meds, for the first time in his life he found himself ignoring deadlines. Once or twice, that had caused difficulties. He bought a Mercedes on the medication. He had always wanted a Mercedes, but off of the medication he considered it a budget buster and foolish.
Mr. K’s case is noteworthy not only because his judgment was altered by the SSRI, but because, at ten months, when we first tried stopping the meds, he would have seemingly illustrated the statistics often replicated in studies, of patients who have a recurrence without their meds, thus providing one more piece of evidence, seeming to confirm the life long implied biological basis of his illness.
But, at 16 months, with the apparent cause of his depression eliminated (his critical supervisor), he did just fine without an SSRI. This doesn’t diminish the almost miraculous effectiveness of his original meds, or that they may have helped him gain the initiative to find a new job, or that he might get depressed again some time in the future. However, it does highlight the kind of questions that clinicians should ask themselves about the particulars involved in a specific patient’s illness, as opposed to exclusively focusing on the operative factors in a specific diagnosed illness. This perspective is in contrast to the clinical practice guideline issues by the U.S. Department of Health and Human Services which flatly states that where there has been a prior episode(s) of major depression “maintenance of antidepressant medication treatment should be for at least one year” 17 Statistically this assertion may have a basis for a population of patients but surely there are circumstances when this “rule” should not guide us. The fact that on follow up recurrences are found so frequently in unmedicated, as opposed to medicated, patients does not automatically demand continued treatment with meds. Generally speaking, the issues involved in a depression are deeply woven into a patient’s character or the fabric of his life. Miraculous transformations are the stuff of melodrama not reality. One would not expect a change in the original factors that led to depression eight months or nine months into treatment, or even years later unless the patient or his circumstances changed. Hence, depression is going to recur off of meds and it is a good idea to continue them. But , this does not have to be the case. There can be a dramatic change in circumstances. If a patient has gone into a deep depression because of financial hardship after he/she has been fired from a job, chances are that finding a new terrific job will very effectively keep depression from recurring. Winning the lottery works even better. The same can be said for a person who does not have a neurotic pattern of relationships, who has gone into a depression after being rejected by a spouse or lover. Finding a new mate works wonders whether it is three months or two years after medication was begun. The perspective being presented here also applies when medication is not involved, for example evidence based treatment using cognitive behavioral therapy.18
A sixteen years old teenager was evaluated for medication for depression. As a young child he was abandoned by his biological mother and raised by his grandparents. His grandmother/mother had died two years before at the age of 74 after her third stroke. His 79 year-old grandfather had severe emphysema, and judging by his labored breathing in the waiting room, didn’t look like he was too long for this world either. At his prep school the patient kept talking about death. Like others when they are depressed, his dark moods didn’t make him very popular with the other students at school, which made him even more depressed. On the basis of his depression diagnosis, his therapist was utilizing cognitive behavioral therapy. Attempts were being made to replace his negative thoughts with positive thoughts through homework exercises.
Although I am a non-believer I would have had no problem if he was being comforted by religion, if he was given a positive way to think about death, for example, that his mother was in heaven, and he would one day see her there. But being told to repetitively practice not thinking about death, replacing it with more positive thoughts by doing homework assignments again and again to accomplish this, places psychiatric cure on the level of its behavioristic antecedents, training rats to perform a task through repetitive exercise.
Is planning the treatment of a 16 year old boy, upset by the death of his mother, and the impending death of his father, best conceptualized with blinders worn by the doctor, that eliminates every non scientific consideration? If a boy, about to become an orphan, had asthma, a pulmonologist could properly focus on the asthma alone and leave ministrations of his soul to a priest. Must this be the position of psychiatrists? The cognitive behavioral therapy offered him, while scientifically sound, was alienating him from the reality of his experience. Fine, given his situation and personality he wasn’t going to be very cheerful. But he might be able to learn to love the blues, or read authors who have come to terms with the death of a loved one, or find friends who like to visit sad territory, or be helped by a therapist who wants to visit him in his own experience, who might legitimize his “negative” feelings and bring dignity to his suffering. Is a doctor who conceptualized the issues this way no longer practicing medicine because he has left the realm of diagnostic psychiatry and clearly defined symptoms? It isn’t that evidence based treatment based on medication trials, or cognitive behavioral shouldn’t be considered, it is that these other clinical issues cannot be addressed unless they are conceptualized. Van Praag’s description of tunnel vision resulting from an exclusive focus on nosology is exactly the point here. Indeed, once a month 15 minute med checks (which may be all that is necessary when practicing evidence based, symptom vs side effect psychiatry) can lead to practitioners being blind to clinically crucial observations. Indeed, laymen described the “well-whatever effect” long before it was addressed in the literature. Consider this ad for a t-shirt.
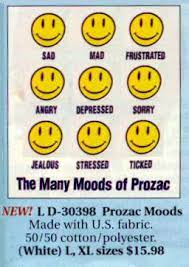
How is this possible other than the “experts” have had their eyes closed to the obvious. They do not know their patients well enough to observe what is apparent to others. Diagnoses, described symptoms for that diagnosis, and the alleviation of this is all that matters.
Brainstorming: Further perspectives and unusual uses of drugs resulting from a psychological rather than diagnostic point of view
SSRIs, and bupropion are believed to be roughly equal in their antidepressant efficacy. But while each stimulates neurotransmitters to give a positive ring to the day, they do not induce the same psychological profile, since rather than effecting serotonin, bupropion acts primarily by enhancing dopamine, and to some extent, norepinephrine. It tends to be activating rather than calming. Most clinicians use bupropion in depression when anergia or anhedonia is prominent, and tend to avoid it if anxiety or agitation characterize a depression. Not surprisingly, it is one of the few antidepressants that hasn’t proven to be effective with panic disorder. It can give an edgy feeling, which, in an already nervous person, can set off panic attacks. But here is the important point for clinicians. There are no hard and fast rules. There are as many exceptions as rules. Guidelines based on the general can serve as starting points, but eventually the particulars are more important, especially when all is not going as planned.
When Mr. K., a 50 year old businessman, transferred to my care, he was already on bupropion for panic disorder. Since this was not indicated for that diagnosis I took him off it. His condition worsened so he was put back on it and he did well. It look the better of 8 or 9 months in weekly psychotherapy sessions before I came up with a plausible explanation. It wasn’t that his brain chemistry was different than others so that bupoprion effected his brain chemicals differently ( a speculation that a chemotherapy oriented psychiatrist might assume). I thought it more likely, after I got to know him better, that bupropion helped his panic attacks for reasons particular to his story.
His mother, during a bohemian interlude in her 20s, had left Connecticut and gone to live in Greenwich Village. New York suited her well. She was attractive, charming, energetic and intelligent. There she met, fell in love with, and married Mr. Ks father, a good looker but a ne’r do well charmer and, it turned out, alcoholic. It didn’t take long for the honeymoon to evaporate. After six or seven years, his mother’s trust fund proved inadequate to support the two of them and their two sons, ( Mr. K and his brother). After many discussions, promises to change, and falling off the wagon Mrs. K’s mother left Mr. K’s father, and returned to her family in Connecticut a broken prodigal daughter.
She soon was resuscitated. Having learned her lesson, she met and married the opposite kind of man. Unlike, Mr. K’s true father, a bohemian a moral relativist, taking great satisfaction poking holes in the hypocrisy and inconsistencies of conventional rules of behavior, his new father stayed on the righteous path of responsibility to the community, and to Christian ideals. He paid unwavering attention to good intentions. Straying from the path, was forever tempting and adventurous compared to the boredom of sticking to what is expected. But the interesting is not always relevant. Christ suffered to relieve the faithful of sin. Mr. K did not cash in on this gift. He preferred to follow Christ’s example. It took supreme effort. Sufffering was proof enough that you were going about things as Christ might have. His new father lived by the book. He loved books. He taught at a very respectable prep school where he took his place alongside other respectable teachers those charged with setting an example for the sons of wealthy families. The lure of no monthly child support checks, allowed Mr. Ks biological father to give up all parental rights so, along with his brother, Mr. K was adopted by his mother’s new husband. And so his only contact with his father, was hearing about his father irresponsible behavior from his new father who could cluck insistently when his father’s name was mentioned.
After the blush of their early romance, his parents settled into real life. The atmosphere was tense. There were some nice things. He could cut a nice figure when he was in a good mood. His mother had chosen her new husband, because of her attraction to him, but it turned out., as in most marriages, physical magnetism hindered clarity of vision. She found his tight ass rule irresistible. And as she had done through earlier incarnations of her unleashed demons, she was a mighty opponent. She asserted her independence in many nice ways, but in the end it was driven by a nasty side of her, that led to symptoms. Secretly she took laxatives, to keep herself stylishly thin. She did well. This time around, she was perfectly presentable to the community, to her husband’s world of headmasters, and fellow teachers. But in the privacy of her castle, she almost constantly had gas, which for comfort often had to be released wherever she was in the house. Several times she had to be hospitalized for her mysterious colonic illness. It took 25 years for her laxative abuse to be discovered, long after my patient had left home.
Mr. K’s adopted father was a perfectionist of the worst variety, stern and unforgiving, and when pushed by my patient’s childish half effort, he was capable of furious outbursts. Not all of this was earned by his misbehavior. In reconstructing the probable scenario in therapy, we thought it very possible that both he and his brother were easier targets than their mother. She, after all, was sickly. Mr K’s adopted father could be friendly to the young. He coached the prep school’s soccer team with passion. He was extremely stern here too. He would scream at his players’ screw-ups, give them the cold eye, or devise some other form of torture. However, he enjoyed soccer and this enjoyment was infectious. Most of those he coached considered him tough, but over all, a good experience. His father’s relationship however to non sport related work was completely different. As with most people it wasn’t a lot of fun, but here his neurotic patterns let loose the full fury of his frustration. As Marlon Brando in On the Waterfront put it, and tens of millions working stiffs since and forever after, have put it, when youth and its possibilities has passed them by: He could have been someone, been a champ. He had been off to a good start, before the army and World War II took him away from his career. It never got going again, not like his brother who had had a fantastic career. He told himself that he chose teaching because of his desire to do some good, to make a difference for other people. He made sure this wasn’t a cop out, wasn’t simply a flight from the battle field, by dedicating his life to hard labor. It wasn’t just his admiration for Christ and wish to be like him. He brought the battlefield with him. He heaped on the challenges, took second and third helpings of things he hated to do. He took pride in this stoicism.
His father’s greatest contempt was reserved for slackers. When they didn’t do their job it meant twice as much for him. He felt sorry for himself because of all of the unrewarded work life dumped on him. The work was never done well enough and never done which made all of his life gruelingly hard. Mr. K and his brother, as children, were kids, champion slackers. The choice between play and work was not difficult. Both knew to get out of the room when their father was in a foul mood, especially if he had been drinking. When he was given an assignment at home Mr. K quickly learned that no matter how well he did it, his father would be dissatisfied, sometimes very dissatisfied, on more than one occasion furious exploding over a mistake, or half effort. God cursed Adam and the human race with have to work with the sweat of their brow. The chain of command (the curse of work) has since been extended from father to son generation after generation, none more so then from stepfather to stepson.
Even if briefly he pleased his father, it never lasted. We speculated that his father’s bitterness and disappointment with his stymied career fanned the flames of any hatred his father felt toward his adopted sons (my patient and his brother). There is a good chance that his father’s drinking grew out of proportion to all of it, to financial stresses not adequately covered by his salary and Mr. K’s mother’s trust fund.
Schoolwork was the worst, whenever Mr. K’s intelligence was challenged. His father seemed to take particular pleasure demonstrating how smart he was and how stupid my patient was, perhaps because he still wanted to prove to Mr. Ks mother that she had made a smart move choosing him and not Mr. K’s biological father. Or perhaps, as noted, it was a way of getting even with his disappointing wife These theories about his parents’ motivations cannot be proven with scientific certainty. (They are a mix of speculation and likelihood. They are offered as an illustration of the kind of thinking that might go on during insight therapy.) In high school, having been compared to him repeatedly, Mr. K soon resembled his biological father. He goofed off, got high on pot, alcohol, and acid. He faked it whenever he ran into a bump in the road, homework that demanded intellectual effort. If it didn’t come effortlessly, it meant he wasn’t smart enough to understand it. This reinforced his adopted father’s characterization of him as a loser/slacker. . Back then ADHD and doctors were not the solution to Mr K’s soon to be disintegration of effort. By not making the effort, he didn’t have to face the possibility that his father was right. He was dumb. It was a self defeating strategy. By giving up early when challenged by difficulty, he wasn’t able to prove to himself that he had the intellectual capacity, to overcome the problem. Most children aren’t sure they have much in the brain department . Not trying and not getting good grades , reinforces the original fear. He was as his father saw him, dumb, a loser. By the time he was in high school he feared, he might fail out of school even if he tried. So try he didn’t. Because of his rule breaking, drug abuse, and failure to do assignments, he was asked to leave the prep school his father taught at. It left an indelible mark on his identity. In later years, through AA, regular church attendance and conformity to a persona that would have made his now dead adopted father proud, he achieved respectability.
There was only one problem. His panic attacks. The first one occurred after a rare visit, when he was 18, to his biological father. His father had actually prospered. After a week together he was driving home in the new car his father gave him, feeling great about himself, great about his car, probably great about the revenge this might exact on his adopted father. It was then that his first panic attack occurred. He was to have several of these throughout his life, whenever he was feeling terrific over his purchase of a new car. Apparently he was terrified of what victory against his father might bring. He was no match for his father’s rage. That much had been branded starting from three and four years old. You didn’t want to get him too angry. There were other dynamics that evolved out of the above framework. If he could put off the pain, offend no one, make promises that he would come through, he’d be safe for a while. This meant regularly promising more than he could deliver. He did it (in the heat of the moment) to be nice, or because he was too afraid to ask for assistance when he didn’t know how to do something. When there were expectations at work beyond what he believed were his capacities, he was in real trouble. As a deadline date approached, the pressure mounted and mounted. It turned out that his panic was related to a fear that the sh’t was going to hit the fan, a panic that his laziness, incompetence, and dishonesty would be discovered. As it had time and again with his father. He had been terrified then and was terrified now. As a dopamineric agent, the bupropion helped him to get things done, thus alleviating the source of his anxiety and panic. It gave him the confidence to forge ahead, an expectation that he was going to accomplish what he had set out to do and take pleasure doing it. His results weren’t guaranteed to be good when he was influenced in this way by the medication, but it didn’t matter. It was his positive expectations. If we recall, his father was equally perfectionistic when he coached soccer, but because he was having a good time, my patient (and his team mates had a good time.) It put my patient in a different psychological mode. Like many fathers and sons, whatever tensions might build up during their lifetimes, sports was the one area they could enjoy each other. Interestingly, Mr. K, well into his 40’s, continued to play and coach soccer, capable of great effort and failures, but with a pleasure that forgave all shortcomings. It worked far better at getting work done than a grinding adherence to the work ethos.
Bupropion seemed to put him in a mode where work he customarily slacked off on became easy, half challenging, sometimes stimulating. This should not be a total surprise. Bupropion is often used in the treatment of depression to augment SSRIs when anhedonia remains. This seems to be a general characteristic of dopaminergic medicines. In the 19th century another dopaminergic agent, cocaine was the most popular miracle drug in the world, regularly used and extolled by the likes of President McKinley, Queen Victoria, Pope Leo Xlll, Thomas Edison, Robert Lewis Stevenson, Ibsen , Anatole France and a host of other renowned members of society. 19 Sigmund Freud wrote the following about it, “You perceive an increase of self-control and possess more vitality and capacity for work. 20 According to the Sears, Roebuck and Co. Consumers’ Guide (1900), their extraordinary Peruvian Wine of Coca “…sustains and refreshes both the body and brain….It may be taken at any time with perfect safety…it has been effectually proven that in the same space of time more than double the amount of work could be undergone when Peruvian Wine of Coca was used, and positively no fatigue experienced.” Nothing has changed. Here is a headline and blurb from the New York Times 21 regarding the effect of stimulants and amphetamines:
“Latest Campus High: Illicit use of Prescription Medication, Experts and Students Say” “Ritalin makes repetitive, boring tasks like cleaning your room seem fun” said Josh Koenig a 20 year old drama major from NYU. “Katherinen Plyshevsky, 21, a junior from New Milford NJ majoring in marketing at NYU said she used Ritalin obtained from a friend with ADD to get through her midterms “It was actually fun to do the work,” she said.
We might also note the new arguments being made for the legitimacy of performance enhancing drugs similar to the stimulants students have found helpful What is the difference between tasks that are experienced as drudgery and those that are satisfying? It is a key question because students diagnosed with ADHD, presumably unable to attend to tasks because of a biological deficit, have no problem paying attention when they are having fun. Many can sit for hours with video games that require extraordinary focused attention. Why does their supposed biological attention deficit not operate here? I evaluated a student who told me that his mind completely fogged over when he had to read something for school. Without his medicine he could go over a page a hundred times and absorb nothing. “Really?” I asked, “You aren”t able to read anything?” “Well,” he told me, “there is one exception.” He was totally into mountain biking. Each month his mountain biking magazine arrived and he devoured that without medicine. Also supportive of this argument-unique charismatic teachers, who make educational material fun, can sometimes succeed with these students. Hence the effectiveness of amphetamines and Ritaline.
Besides ADHD diagnosed adolescents, and their friends, who sometimes borrow their meds when they have to do chores that they dread, stimulants (“greenies”), according to David Wells22, and more recently Mike Schmidt 24have long been part of the professional athletes’ equipment, helping them to step up to the plate with confidence. It changes their state of mind from a passive, reactive, position to a take charge proactive stance. Or as one basketball player put it, “Give me the ball. I can make the shot.” This taking charge, “I can do it” feeling, when approaching tasks, is a key element in most people’s perception of whether they are up to a challenge, and whether it is “work” or pleasurable.
A patient reported to me that one of her employees decided, on her own, that their showroom needed a new paint job. My patient wasn’t sure if this were true, or if she liked the color of paint chosen, but she didn’t object. She came in one day and it was done. Her employee had done a terrific job. If my patient, who was her boss, had asked her to paint the showroom, the reaction would have been, “You have to be kidding. I am not a painter.” It has something to do with the idea, the inspiration coming from her employee. Hence her consequent enthusiasm to make her point. Observe the new owner of the local diner. He will work ten, twelve, fifteen hours at a clip. He will polish the windows, try to improve the menu, rearrange the napkin holders, move from project to project always with energy to spare. Unless he has a gift for management his teen age employees will be moving along at a snail’s pace, keeping one eye on the clock. They will go home more tired than the boss.
Dopaminergic drugs help you feel like the boss. They make you feel in charge. They make you feel like reward will be assured. They make arduous tasks easy. It was not just Mr. K. I soon learned bupropion seems to often be effective for anxiety whenever, in a patient’s psychology, it was connected to not getting things done, when, chores hang over the patient, as both dreaded tasks, and dastardly consequences will ensue if the work isn’t done. When they get the work done the anxiety diminishes. So a drug that at first glance might be expected to make a patient edgy works against anxiety in those with this particular dynamic. My off the cuff guess is that this dynamic is not particularly common in panic disorder.
Mr Ks case was unique. Bupropion could never become an “evidence based” treatment for panic disorder, but like our example of thyroid hormone in CHF it made perfect sense in Mr. Ks case and others with that kind of conflict. It is probably not uncommon in Generalized Anxiety Disorder, but most likely, patients with this relationship to getting work done make up a minority of cases. As noted, dopaminergic drugs makes sense in a large number of children and adolescents with ADHD because there has been a failure to bond, and identify with parents’ and teachers’ expectations.
Children without ADHD, to a much greater extent, have incorporated into their bond with their parents (and later authority figures) the satisfaction and sense of self initiative when they are asked to do something to please (or not disappoint) them. It is far from perfect but compared to children (or adults) with ADHD, for whom almost any expectations are experienced as drudgery, boredom in the classroom is assured. In that case, their behavior is exactly what could be expected from any bored trapped child, daydreams and restless fidgetiness, trying to liven thing up to suit their need to not feel at the mercy of the situation. Doing what they want, including making noise, gives them the feeling that they are in charge of their experience. It may get them in trouble, but they are not passive, not vanquished.
How much simpler to supply this feeling through stimulants. Thus, instead of stimulating hyperactive qualities, the stimulant becomes calming by making the work pleasurable instead of oppressive. It does not addresses the core problem, the child’s failure to bond with authority figures, or group norms, or transform expected behavior to comply with another’s will, so that they feel like an active participant when obeying. But it is not a bad approximation The key issue is searching for a connection between symptoms and psychological issues rather than assuming biological causality of a DSM IV diagnosis explains the problem. I have applied this thinking to certain causes of anxiety, and the behavior of children when they are not responding well to tasks, but the same kind of approach offers opportunities in many areas of psychopathology. For example, like patients with obsessive compulsive personality (as well as many with OCD) like Mr. K’s father, often experience their life as continually oppressive, essentially filled with exhausting never ending chores. With every bit of his strength, Sysyphus, had to push his boulder to the top of the hill, then it would roll back to the bottom and he had to begin again. His punishment went on forever. For patients with this curse there is no end to it unless they die and “rest in peace,” or become disabled and receive government checks for their bad backs. Unlike those with ADHD they perform tasks (begrudgingly), or attempt it, or intend to attempt. Their to-do list never gets done. They cannot deal with the shame associated with goofing up. One way or another, whatever they actually do, the conflict preoccupies and exhausts them. Resentment of those who don’t work as hard as they do is inevitable. Like Mr. K’s father there may be fury at their adolescent children who don’t pitch in, or spouses, or partners in business. Joffe24 found that amphetamines can help OCD. SSRIs allow obsessive patients to soften their sense of imprisonment from their injunctions. They can let some of them go.
In those obsessive patients where I have tried bupropion (I have not yet tried to use stimulants for obsessive symptoms) as expected, it seemed to make work less oppressive, sometimes make it seem, as noted above, easy and “fun.” In two cases, when I used it in this context, some of their anger seemed to diminish (as well as their guilt and feelings of worthlessness for their mysterious unacceptable (often consciously denied) hatred/ anger. Once again I did not make the decision on the basis of diagnosis, but when their resentment over duties, bubbled furiously into the sessions, we went with the bupropion. Case after case can be cited, where this kind of thinking can be productive, serving as a rich source of hypothesis and hunches that might provide a therapeutic dividend, but we will end with a very unusual use of medication. Once again, it is understandable when the psychological issues are considered.
A patient with PTSD for over ten years presented on high doses of Adderall that had been given to him for what his family physician diagnosed as adult ADHD. (He had reported difficulty concentrating.) His physician then became uncomfortable administering stimulants and sent him to me. His history revealed that he did not have ADHD. But he reported that on the Adderall his post traumatic stress disorder was the best it had been in over a decade. It took a while to make sense of this but once again the explanation appeared to be found in his history. He and his fiance had been trainees at a state police academy. His fiance committed suicide with her gun, blowing her brains out. My patient found her body. He couldn’t clear his mind of the scene. During the day, during his dreams, her brain and skull fragments on the wall remained vivid. To make matters worse, he became a paramedic working on an ambulance which brought him to car crash scenes where horribly damaged bodies were not infrequent. Eventually in therapy 5 years before he came to me, he realized this was not good for him, and for years he had worked on a hospital ward. Even with SSRIs and benzodiazepines, his PTSD not infrequently took control of his mind. This no longer happened with the addition of Adderall.
My guess was the Adderall brought back his pre-morbid, state policeman defensive structure. Instead of experiencing his trauma again and again as a helpless passive victim, the essence of the psychological position occupied by those suffering from PTSD, on the Adderall he had returned to being a take charge kind of guy. Coincidentally I was also seeing another patient with PTSD. She was a drug salesman who had been a work out nut. She spoke in short staccato sentences. Boom boom, bam bam, not a trace of sentimentality in her, not a soft syllable in her repertoire. She had been in a car accident and broken her collarbone, right arm and one of her legs. She couldn’t work out. She kept re-experiencing her helplessness in the accident. She was on SSRIs which were helpful but not curative. The addition of Adderall worked like a charm.
Like the other examples, this is not an endorsement of Adderall for PTSD. It is an endorsement for this kind of thinking in formulating cases where this might be helpful. We are not talking about psychoanalytic understanding being necessary, but it does require training to think psychologically in a productive way. The treatments described will not prove efficacy to a scientist’s satisfaction. Moreover, some, or all of these formulations may turn out to have been wrong. But it throws down a challenge. These ideas are only a fraction of what might be possible if others were thinking this way. This should be encouraged. Psychiatric journals should be publishing ideas on subjects like these, so that we can discuss and brainstorm, and end the monopoly that DSM IV and scientific psychiatry has imposed on legitimate practice and discussion. Our experts should weigh in on these issues. Hopefully, one day our patients will be effectively treated by a psychiatry entirely based on science. However, we are far away from being there. Until we have the knowledge to practice in that way, we are doing a disservice by making believe we scientifically know what we do not, and ignore faculties we possess, or that lively discussion and training can improve. It might be helpful to our patients.
References and notes:
1. Ruh” HG, Huyser J, Swinkels JA, Schene AH, Switching antidepressants after a first selective serotonin reuptake inhibitor in major depressive disorder: a systematic review J Clin Psychiatry. 2006; 67:1836-55.
2. Nierenberg AA, Keefe BR, Leslie VC, Alpert JE, Pava JA, Worthington JJ 3rd, Rosenbaum JF, Fava M Residual symptoms in depressed patients who respond acutely to fluoxetine. J Clin Psychiatry. 1999; 60:221-5.
3. Baghai, TC, Moller, HJ, Rupprecht, R. Recent progress in pharmacological and non-pharmacological treatment options of major depression. Curr Pharm Des.2006; 12: 503-15
4. Papakostas GI, Fava M, Thase ME Treatment of SSRI-resistant depression: a Meta-analysis comparing within- versus across-class switches. Biol Psychiatry. 2008; 63:699-704
5. S. Kendler, M. McGuire, A. M. Gruenberg, A. O’Hare, M. Spellman and D. Walsh The Roscommon Family Study. III. Schizophrenia-related personality disorders in relatives Arch Gen Psychiatry Vol 50 No. 10 Oct 1993
6. Mareno,C, et al “National Trends in the Outpatient Diagnosis and Treatment of Bipolar Disorder in Youth” Arch Gen Psychiatry 2007:64 (9): 1032-1039
7. Mahmoud et al.( 2007) Risperidone for Treatment-Refractory Major Depressive Disorder: A Randomized Trial Ann Intern Med.; 147: 593-602
8. Fava M, Rush AJ, Alpert JE, Balasubramani GK, Wisniewski SR, Carmin CN, Biggs MM, Zisook S, Leuchter A, Howland R, Warden D, Trivedi MH. “Difference in treatment outcome in outpatients with anxious versus nonanxious depression: a STAR*D report” Am J Psychiatry. 2008 Mar;165(3):342-51. Epub 2008 Jan 2.
9. Vonpraag, H. Nosological tunnel vision in biological psychiatry. A plea for a functional psychopathology Annals of the New York Academy of Sciences, 1990; 600 : Issue 1 501-510
10. Detke MJ, Rickels M, Lucki I (1995) Active behaviors in the rat forced swimming test differentially produced by serotonergic and noradrenergic antidepressants Psychoparmacology (Berl) 2006; 121 (1):66-72
11. Oliver B, Molewijk E, van Oorschot R, et al., New animal models of anxiety. Eur Neuropsycho-pharmacol 1994; 2:93-102
12.Pomerantz, J Loss of Appropriate Anxiety: An SSRI Overmedication effect? http://pharmacotherapy.medscape.com/SCP/DBT/1999/V11.n10
13. Franz,B (as reported by Sherman, C) Adjunctive Oral Morphine Effective for Refractory OCD Clinical Psychiatry News 2001; 7: July 29 4
14. Are we acting as doctors if we treat a condition that is not an “illness?” Should medical insurance cover treatment of a condition that is not an “illness?” Or should DSM describe adolescent turmoil as a condition with full understanding that narrowly defined efficacy studies aren’t particularly helpful? The key issue is that psychopathology is being addressed regardless of diagnosis. We might even get better diagnostic thinking if clinicians didn’t have to fabricate DSM conditions to suit insurance forms, and parity regulations.
15. Previously, I have cited other lengths of time in describing this but after reviewing my notes this is the accurate time period
16. Shapiro, D Neurotic Styles Basic Books 1965
17. Clinical Practice Guideline, Depression in Primary Care: Detection, Diagnosis and Treatment, US Department of Health and Human Services, Agency for Health Care Policy and Research, Washington DC, Quick Reference Guide for Clinicians Number 5, April 1993
18. Sobo, S. On the banality of positive thinking Psychiatric Times 2001;
19. History and uses of the Coca leaf” http://www2.truman.edu/~marc/webpages/andean2k/cocaine/history.html
20. The Life and Work of Sigmund Freud, Volume I (1856-1900) (New York: Basic Books, 1953), p. 82-83
21. Latest Campus High: Illicit use of Prescription Medication, Experts and Students Say:” NY Times Page B8 3/24/00
22. Wells, D. and Kreski, C. (2003) Perfect I’m Not: Boomer on Beer, Brawls, Backaches, and Baseball. New York: William Morrow
23. Schmidt, M. (2003) Clearing the Bases. New York: HarperCollins
24. Joffe, Russell t. MD; Swinson, Richard P. MD; Levitt, Anthony Acute Psychostimulant Challenge in Primary Obsessive-Compulsive Disorder Journal of Clinical Psychopharmacology. 11(4):237-241, August 1991.
25. Kaplan, Arlene DSM-V Controversies Psychiatric Times v26 p1 January 2009
26. A Warning Sign on the Road to DSM V Alan Frances M.D., chair of the DSM IV Task Force has this to say about DSM V which is promising all kinds of dramatic improvements in diagnosis: “There can be no dramatic improvements in psychiatric diagnosis until we make a fundamental leap in our understanding of what causes mental disorder. The incredible recent advances in neuroanatomy, molecualar biology, and brain imaging that have taught us so much about normal brain functioning are still not relevant to the clinical practice of everyday psychiatric diagnosis. The clearest evidence supporting this disappointing fact is that not even a single biological test ready for inclusion in the criteria for DSM-V” Concerning the “paradigm shift that might occur of basing diagnosis on biological findings.” he write ” Unfortunately, this is years (if not decades) from fruition.” He continues, “Descriptive diagnosis should remain fairly stable until disorder by disorder, we gradually attain a more fundamental and explanatory understanding of causality. Later he notes “There is also the serious, subtle, and ubiquitous problem of unintended consequences. As a rule of thumb, it is wise to assume that unintended consequences will come often and in very varied and surprising flavors. For instance, a seemingly small change can sometimes result in a different definition of caseness that may have a dramatic and totally unexpected impact on the reported rates of a disorder. Thus, are false “epidemics” created. For example, although many other factors were certainly involved, the sudden increase in the diagnosis of autistic, attention-deficit/hyperactivity, and bipolar disorders may in part reflect changes made in the DSM-IV definitions. Later he writes: ” This issue becomes particularly relevant when one considers the skillful pressure likely to be applied by the pharmaceutical industry after the publication of DSM-V. It has to be assumed that they will attempt to identify every change that could conceivably lead to a marketing advantage—often in ways that will not have occurred to the DSM-V Task Force. To promote sales, the companies may sponsor “education” campaigns focusing on the diagnostic changes that most enhance the rate of diagnosis for those disorders that will lead to the increased writing of prescriptions… there is a great risk of many new “epidemics” based on changes suggested for DSM-V.”
1 comment
Comments are closed.